Table name: COST
The COST table captures all cost information for procedures, drugs, visits and devices.
Key conventions
- Costs will be taken from TEMP_INPATIENT_ADMISSIONS, TEMP_MEDICAL and DRUG_CLAIMS and should be loaded after the VISIT_OCCURRENCE table since the mapped domains will be needed in order to properly associate the costs with the correct fact table (CONDITION_OCCURRENCE, PROCEDURE_OCCURRENCE, DEVICE_EXPOSURE, DRUG_EXPOSURE, MEASUREMENT, OBSERVATION or VISIT_OCCURRENCE).
- Each line of service from TEMP_MEDICAL table will create one and only one record in the COST table since costs are associated with PROC1.
- Starts after you have remove duplicate drug records (see Drug Claims to STEM documentation).
- After mapping each PROC1 in TEMP_MEDICAL to the correct CONCEPT_ID and the correct DOMAIN during the VISIT_OCCURRENCE step, use this information to populate COST_EVENT_ID and COST_DOMAIN_ID.
- When taking cost information from TEMP_INPATIENT_ADMISSIONS we take any INPATIENT_ADMISSION that matches up to an ‘IP’ TEMP_MEDICAL record on ENROLID, CASEID, and YEAR.
- Drug cost information is pulled from the DRUG_CLAIMS table at the same time the DRUG_EXPOSURE is loaded and follows the same pull logic as described for DRUG_EXPOSURE table.
Reading from DRUG_CLAIMS
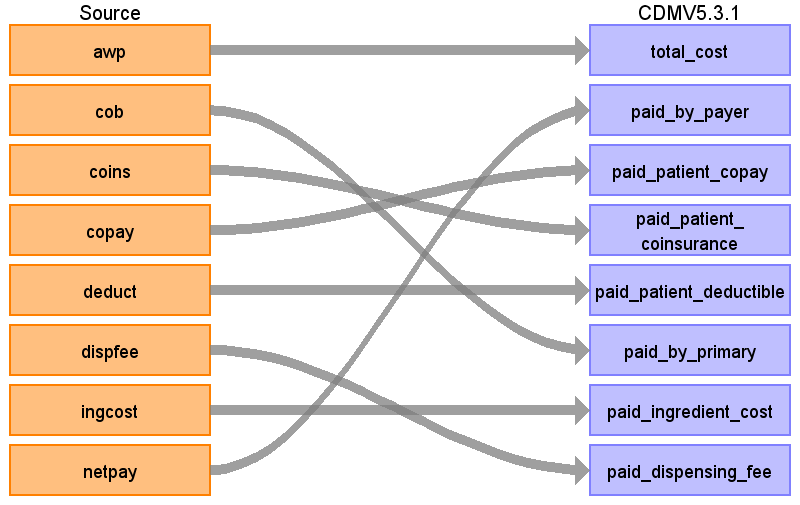
| Destination Field | Source field | Logic | Comment field |
|---|---|---|---|
| COST_ID | - | A system generated unique identifier for each cost record | - |
| COST_EVENT_ID | - | Costs coming from the DRUG_CLAIMS table will have COST_EVENT_ID = DRUG_EXPOSURE_ID | - |
| COST_DOMAIN_ID | - | Drug | - |
| COST_TYPE_CONCEPT_ID | - | 32810 | 32810 Claim |
| CURRENCY_CONCEPT_ID | 44818668 | This will be 44818668 for all rows since this is a US claims database and paid in US Dollars. | |
| TOTAL_CHARGE | - | - | - |
| TOTAL_COST | AWP | - | - |
| TOTAL_PAID | - | PAID_BY_PAYER + PAID_BY_PATIENT + PAID_BY_PRIMARY | - |
| PAID_BY_PAYER | netpay | SUM(NETPAY) | - |
| PAID_BY_PATIENT | - | PAID_PATIENT_COPAY + PAID_PATIENT_COINSURANCE + PAID_PATIENT + DEDUCTIBLE | - |
| PAID_PATIENT_COPAY | copay | SUM(COPAY) | - |
| PAID_PATIENT_COINSURANCE | coins | SUM(COINS) | - |
| PAID_PATIENT_DEDUCTIBLE | deduct | SUM(DEDUCT) | - |
| PAID_BY_PRIMARY | cob | SUM(COB) | - |
| PAID_INGREDIENT_COST | ingcost | SUM(INGCOST) | - |
| PAID_DISPENSING_FEE | dispfee | SUM(DISPFEE) | - |
| PAYER_PLAN_PERIOD_ID | - | - | Lookup associated PAYER_PLAN_PERIOD_ID. Look up by PERSON_ID and PROCEDURE_DATE. If there no match, put NULL. There should only be one possible plan. |
| AMOUNT_ALLOWED | - | NULL | - |
| REVENUE_CODE_CONCEPT_ID | - | 0 | - |
| REVENUE_CODE_SOURCE_VALUE | - | NULL | - |
| DRG_CONCEPT_ID | - | 0 | - |
| DRG_SOURCE_VALUE | - | NULL | - |
Reading from OUTPATIENT_SERVICES
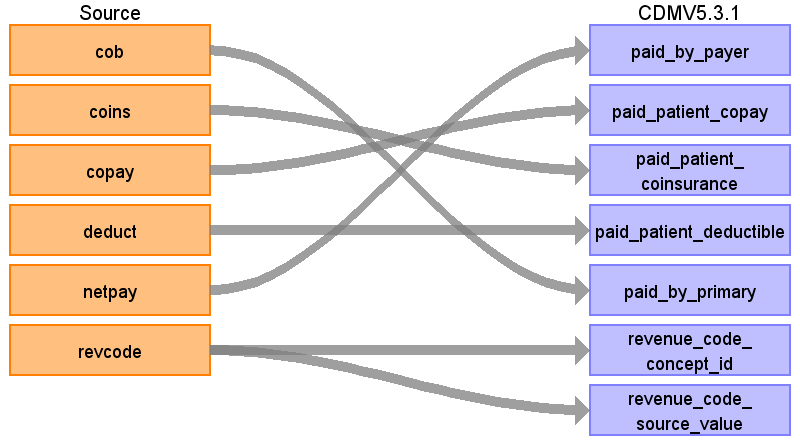
| Destination Field | Source field | Logic | Comment field |
|---|---|---|---|
| COST_ID | - | A system generated unique identifier for each cost record | - |
| COST_EVENT_ID | - | This allows the cost to be linked to the associated record. If a PROC1 code maps to a CONCEPT_ID with a domain of ‘device’, then this will be the DEVICE_EXPOSURE_ID assigned in the DEVICE_EXPOSURE table. | - |
| COST_DOMAIN_ID | - | If a PROC1 code maps to a CONCEPT_ID with a domain of ‘Device’, then this will be ‘Device’. | - |
| COST_TYPE_CONCEPT_ID | - | 32810 | 32810 Claim |
| CURRENCY_CONCEPT_ID | - | 44818668 | This will be 44818668 for all rows since this is a US claims database and paid in US Dollars. |
| TOTAL_CHARGE | - | NULL | - |
| TOTAL_COST | - | NULL | - |
| TOTAL_PAID | - | PAID_BY_PAYER + PAID_BY_PATIENT + PAID_BY_PRIMARY | - |
| PAID_BY_PAYER | NETPAY | - | - |
| PAID_BY_PATIENT | - | PAID_PATIENT_COPAY + PAID_PATIENT_COINSURANCE + PAID_PATIENT + DEDUCTIBLE | - |
| PAID_PATIENT_COPAY | COPAY | - | - |
| PAID_PATIENT_COINSURANCE | COINS | - | - |
| PAID_PATIENT_DEDUCTIBLE | DEDUCT | - | - |
| PAID_BY_PRIMARY | COB | - | - |
| PAID_INGREDIENT_COST | - | NULL | - |
| PAID_DISPENSING_FEE | - | NULL | - |
| PAYER_PLAN_PERIOD_ID | - | Lookup associated PAYER_PLAN_PERIOD_ID. Look up by PERSON_ID and PROCEDURE_DATE. If there no match, put NULL. There should only be one possible plan. | - |
| AMOUNT_ALLOWED | - | NULL | - |
| REVENUE_CODE_CONCEPT_ID | REVCODE | Use the Source-to-Standard Query Filters: WHERE SOURCE_VOCABULARY_ID IN ('Revenue Code') AND TARGET_STANDARD_CONCEPT = 'S' | - |
| REVENUE_CODE_SOURCE_VALUE | REVCODE | - | - |
| DRG_CONCEPT_ID | - | 0 | - |
| DRG_SOURCE_VALUE | - | - | - |
Reading from INPATIENT_ADMISSIONS
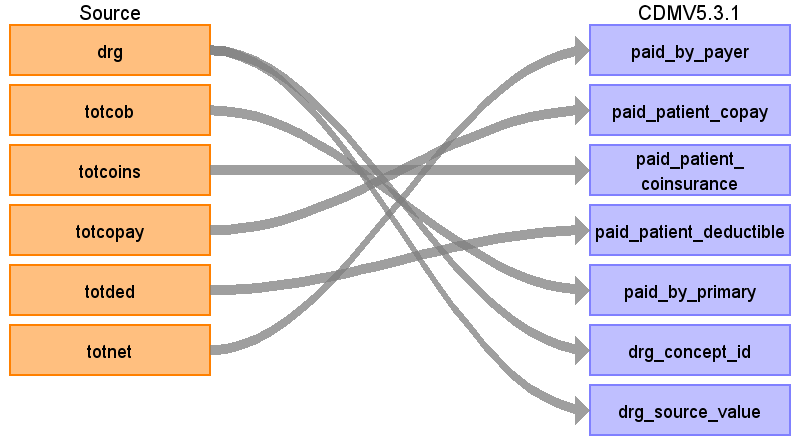
| Destination Field | Source field | Logic | Comment field |
|---|---|---|---|
| COST_ID | - | A system generated unique identifier for each cost record | - |
| COST_EVENT_ID | - | This allows the cost to be linked to the associated record. If a PROC1 code maps to a CONCEPT_ID with a domain of ‘device’, then this will be the DEVICE_EXPOSURE_ID assigned in the DEVICE_EXPOSURE table. | - |
| COST_DOMAIN_ID | - | If a PROC1 code maps to a CONCEPT_ID with a domain of ‘Device’, then this will be ‘Device’. | - |
| COST_TYPE_CONCEPT_ID | - | 32810 | 32810 Claim |
| CURRENCY_CONCEPT_ID | - | 44818668 | This will be 44818668 for all rows since this is a US claims database and paid in US Dollars. |
| TOTAL_CHARGE | - | NULL | - |
| TOTAL_COST | - | NULL | - |
| TOTAL_PAID | - | PAID_BY_PAYER + PAID_BY_PATIENT + PAID_BY_PRIMARY | - |
| PAID_BY_PAYER | TOTNET | - | - |
| PAID_BY_PATIENT | - | PAID_PATIENT_COPAY + PAID_PATIENT_COINSURANCE + PAID_PATIENT + DEDUCTIBLE | - |
| PAID_PATIENT_COPAY | TOTCOPAY | - | - |
| PAID_PATIENT_COINSURANCE | TOTCOINS | - | - |
| PAID_PATIENT_DEDUCTIBLE | TOTDED | - | - |
| PAID_BY_PRIMARY | totcob | - | - |
| PAID_INGREDIENT_COST | - | NULL | - |
| PAID_DISPENSING_FEE | - | NULL | - |
| PAYER_PLAN_PERIOD_ID | - | Lookup associated PAYER_PLAN_PERIOD_ID. Look up by PERSON_ID and PROCEDURE_DATE. If there no match, put NULL. There should only be one possible plan. | - |
| AMOUNT_ALLOWED | - | - | |
| REVENUE_CODE_CONCEPT_ID | - | - | - |
| REVENUE_CODE_SOURCE_VALUE | - | - | - |
| DRG | DRG | Use the Source-to-Standard Query Filters: WHERE SOURCE_VOCABULARY_ID IN ('DRG')AND SOURCE_CONCEPT_CLASS_ID IN ('MS-DRG')AND TARGET_STANDARD_CONCEPT = 'S'AND TSVCDAT >= TARGET_VALID_START_DATEAND TSVCDAT <= TARGET_VALID_END_DATEAND TARGET_STANDARD_CONCEPT IS NOT NULL | The filter to the left should be used for records coming from the INPATIENT_SERVICES table only. When a cost record comes from the INPATIENT_ADMISSIONS table replace TSVCDAT with DISDATE. |
| DRG_SOURCE_VALUE | DRG | - | - |
Reading from INPATIENT_SERVICES
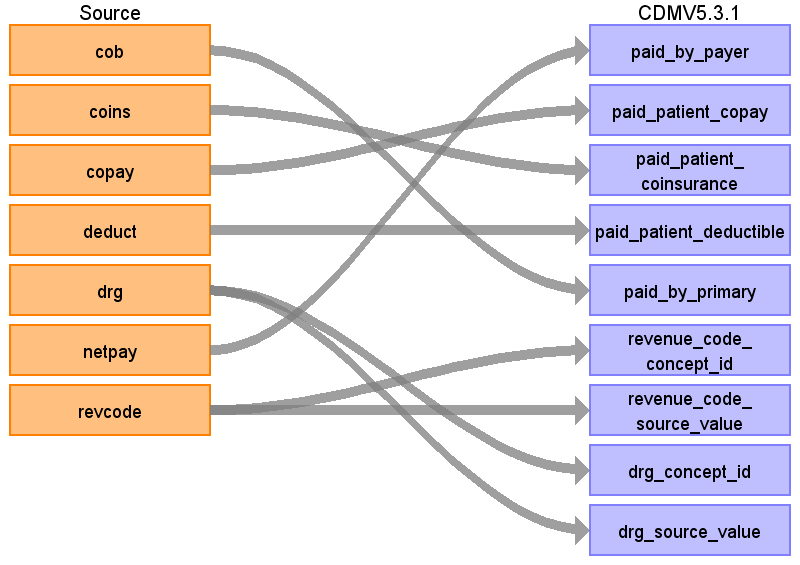
| Destination Field | Source field | Logic | Comment field |
|---|---|---|---|
| COST_ID | - | A system generated unique identifier for each cost record | - |
| COST_EVENT_ID | - | This allows the cost to be linked to the associated record. If a PROC1 code maps to a CONCEPT_ID with a domain of ‘device’, then this will be the DEVICE_EXPOSURE_ID assigned in the DEVICE_EXPOSURE table. | - |
| COST_DOMAIN_ID | - | If a PROC1 code maps to a CONCEPT_ID with a domain of ‘Device’, then this will be ‘Device’. | - |
| COST_TYPE_CONCEPT_ID | - | 32810 | 32810 Claim |
| CURRENCY_CONCEPT_ID | - | 44818668 | This will be 44818668 for all rows since this is a US claims database and paid in US Dollars. |
| TOTAL_CHARGE | - | NULL | - |
| TOTAL_COST | - | NULL | - |
| TOTAL_PAID | - | PAID_BY_PAYER + PAID_BY_PATIENT + PAID_BY_PRIMARY | - |
| PAID_BY_PAYER | NETPAY | - | - |
| PAID_BY_PATIENT | - | PAID_PATIENT_COPAY +PAID_PATIENT_COINSURANCE+PAID_PATIENT+DEDUCTIBLE | - |
| PAID_PATIENT_COPAY | COPAY | - | - |
| PAID_PATIENT_COINSURANCE | COINS | - | - |
| PAID_PATIENT_DEDUCTIBLE | DEDUCT | - | - |
| PAID_BY_PRIMARY | COB | - | - |
| PAID_INGREDIENT_COST | - | NULL | - |
| PAID_DISPENSING_FEE | - | NULL | - |
| PAYER_PLAN_PERIOD_ID | - | Lookup associated PAYER_PLAN_PERIOD_ID. Look up by PERSON_ID and PROCEDURE_DATE. If there no match, put NULL. There should only be one possible plan. | - |
| AMOUNT_ALLOWED | - | - | |
| REVENUE_CODE_CONCEPT_ID | revcode | Use the Source-to-Standard Query Filters: WHERE SOURCE_VOCABULARY_ID IN ('Revenue Code') AND TARGET_STANDARD_CONCEPT = 'S' | - |
| REVENUE_CODE_SOURCE_VALUE | revcode | - | - |
| DRG_CONCEPT_ID | DRG | Use the Source-to-Standard Query Filters: WHERE SOURCE_VOCABULARY_ID IN ('DRG')AND SOURCE_CONCEPT_CLASS_ID IN ('MS-DRG')AND TARGET_STANDARD_CONCEPT = 'S'AND TSVCDAT >= TARGET_VALID_START_DATEAND TSVCDAT <= TARGET_VALID_END_DATEAND TARGET_STANDARD_CONCEPT IS NOT NULL | The filter to the left should be used for records coming from the INPATIENT_SERVICES table only. When a cost record comes from the INPATIENT_ADMISSIONS table replace TSVCDAT with DISDATE. |
| DRG_SOURCE_VALUE | DRG | - | - |